Angle Placement of Resurfacing Components
June 9, 2009
Hi Vicky,
Thanks for sending the x-rays of Patient X who has high metal ion levels.
I am not surprised that there is an epidemic.
In hip surgery the 'safest' in the sense of being accommodative of surgeon's errors is using polyethylene but has the worst performance
The next best is ceramic in the safety issue of surgeon error and is 2nd best on performance
Metal on metal has the best performance but unforgiving on surgical error.
Safety Vs high performance has this inverse relationship in most things in life! Cars & bikes for example)
All the increased ions etc. seen now is completely due to surgical error.
There is a recent article in the JBJS British titled ' The painful hip resurfacing' in which the surgical error being the cause of all metal related problem is very well brought out. (See article below)
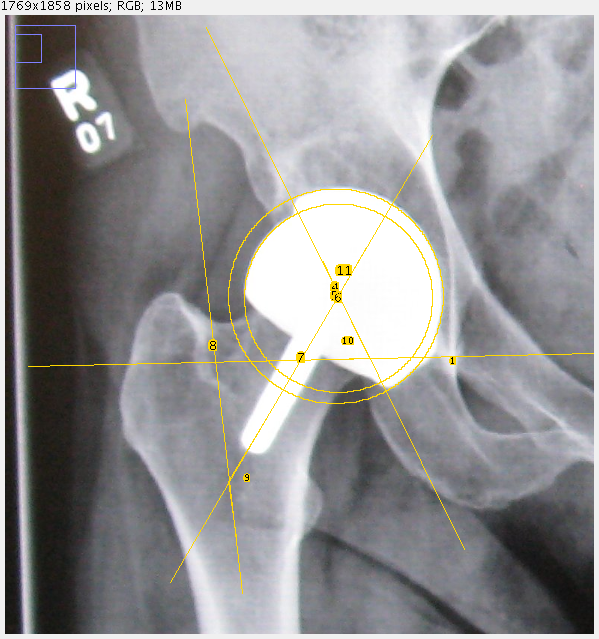
I measured the angles in this patients new x-ray that you sent across(Patient X)
They are as follows: Neck shaft angle :140.28
Acet. Inclination : 65.38
*CAVA : 205.66 (combined abduction - valgus angle) in resurfacings.
This is an angle that I have described and I for which I am writing a paper for publication in the journal of arthroplasty.
The CAVA must be 180 +/- 10 degrees. This is grossly off the mark in this patient (Patient X). Another very important message is that if the CAVA was 195 for example then changing the femoral head to a stemmed component with a stem of a 131 degree neck shaft angle will bring the CAVA to an acceptable range. This of course is very easy surgery taking 20 minutes.
In this patient changing the NSA to 131 by using a stem will not bring the CAVA to an acceptable range. Hence this patient must have a full revision of the cup and the femoral head which is a very major surgical undertaking. However there is no choice and it is better done sooner rather than later.
Again re-emphasizing:
The CAVA angle is very important in resurfacing and is described in our paper on hip resurfacing in AVN that we have submitted to the british JBJS.
The CAVA must be 180+/- 10 degrees. From 10 to 15 degrees is the grey zone. and over 15 degrees is a problem situation.
Journal of Bone and Joint Surgery - British Volume, Vol 91-B, Issue 6, 738-744.
doi: 10.1302/0301-620X.91B6.21682
Copyright © 2009 by British Editorial Society of Bone and Joint Surgery
The painful metal-on-metal hip resurfacing
A. J. Hart, FRCSG(Orth), Clinical Senior Lecturer & Honorary Consultant Orthopaedic Surgeon1; S. Sabah, BSc, Medical Student1; J. Henckel, MRCS, Clinical Research Fellow & Specialist Registrar in Orthopaedics1; A. Lewis, FRCS(Orth), Consultant Orthopaedic Surgeon1; J. Cobb, FRCS, Professor of Orthopaedic Surgery1; B. Sampson, MRSC, CChem, Director of Supraregional Trace Element Laboratory1; A. Mitchell, FRCR, Consultant Musculoskeletal Radiologist1; and J. A. Skinner, FRCS(Orth), Consultant Orthopaedic Surgeon2
1 Department of Radiology Imperial College, Charing Cross Hospital, Fulham Palace Road, London W6 8RF, UK.
2 Department of Orthopaedics Royal National Orthopaedic Hospital, Brockley Hill, Stanmore, Middlesex, HA7 4LP, UK.
Correspondence should be sent to Mr A. J. Hart; e-mail: a.hart@imperial.ac.uk
We carried out metal artefact-reduction MRI, three-dimensional CT measurement of the position of the component and inductively-coupled plasma mass spectrometry analysis of cobalt and chromium levels in whole blood on 26 patients with unexplained pain following metal-on-metal resurfacing arthroplasty.
MRI showed periprosthetic lesions around 16 hips, with 14 collections of fluid and two soft-tissue masses. The lesions were seen in both men and women and in symptomatic and asymptomatic hips. Using three-dimensional CT, the median inclination of the acetabular component was found to be 55° and its positioning was outside the Lewinnek safe zone in 13 of 16 cases. Using inductively-coupled plasma mass spectrometry, the levels of blood metal ions tended to be higher in painful compared with well-functioning metal-on-metal hips.
These three clinically useful investigations can help to determine the cause of failure of the implant, predict the need for future revision and aid the choice of revision prostheses.
For full article click here
http://www.jbjs.org.uk/cgi/content/abstract/91-B/6/738
