Derek McMinn addresses the 4Corners Dispatches program
The Dispatches program 'Going Under the Knife' aired on the 16th of May 2011 and 'The One Show' program aired on the 24th of May 2011 raise two or three important questions.
TV Programs 'Dispatches' and 'The One Show' highlighted failures with ASR resurfacings. Do these apply to the BHR as well?
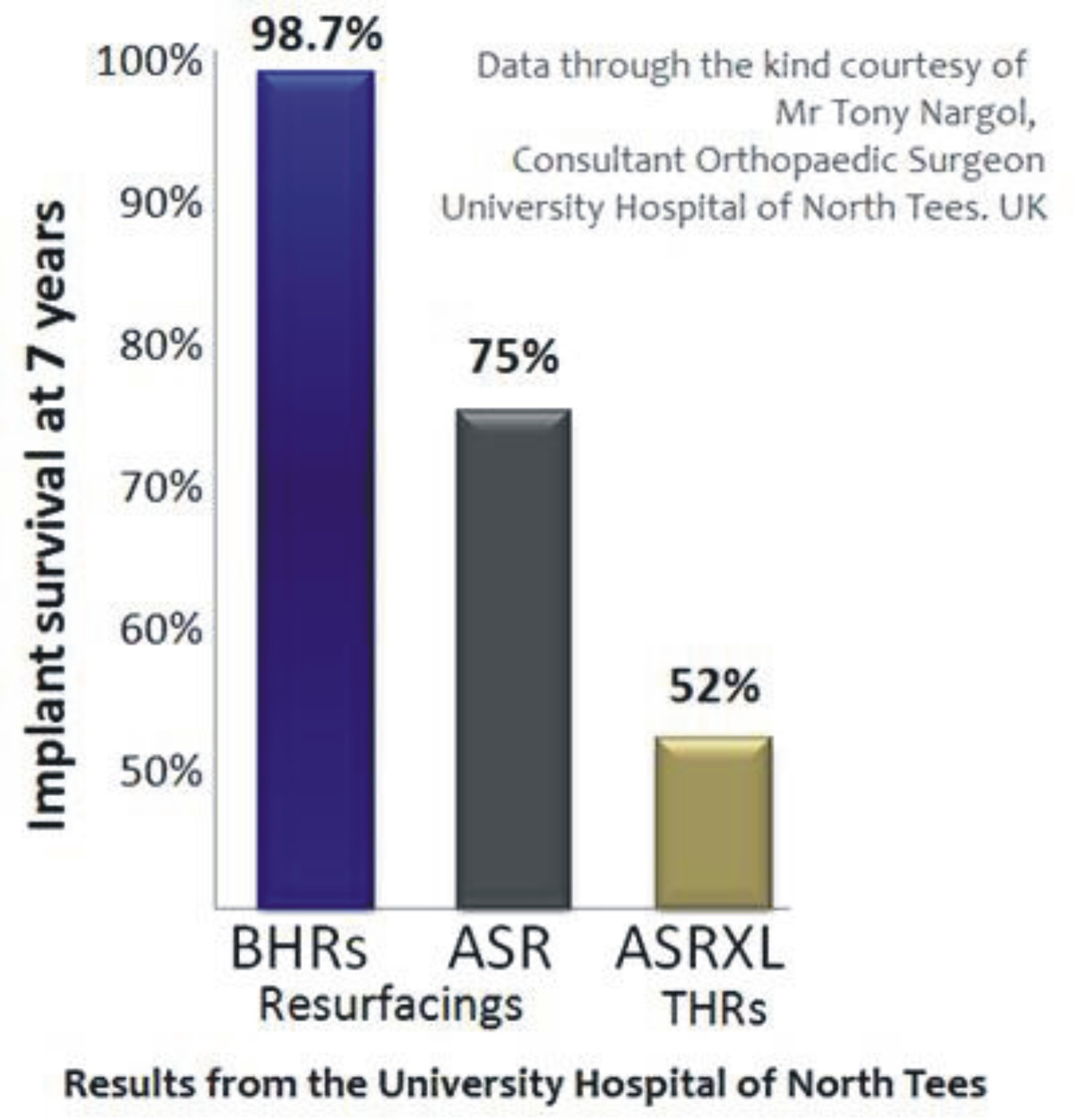
These TV programs did a good job of bringing to attention the sad saga of failures with the ASR hip. Although the experience of only one Centre was highlighted, this experience with ASR failures is widespread. What the programs did not show was the experience of the same Centre with Birmingham Hip Resurfacings (BHR). Their data in the figure below clearly shows that wear‐related failures with the BHR are extremely low (1.3%) and that failures are highly implant specific. BHR is now being used in their Centre again.
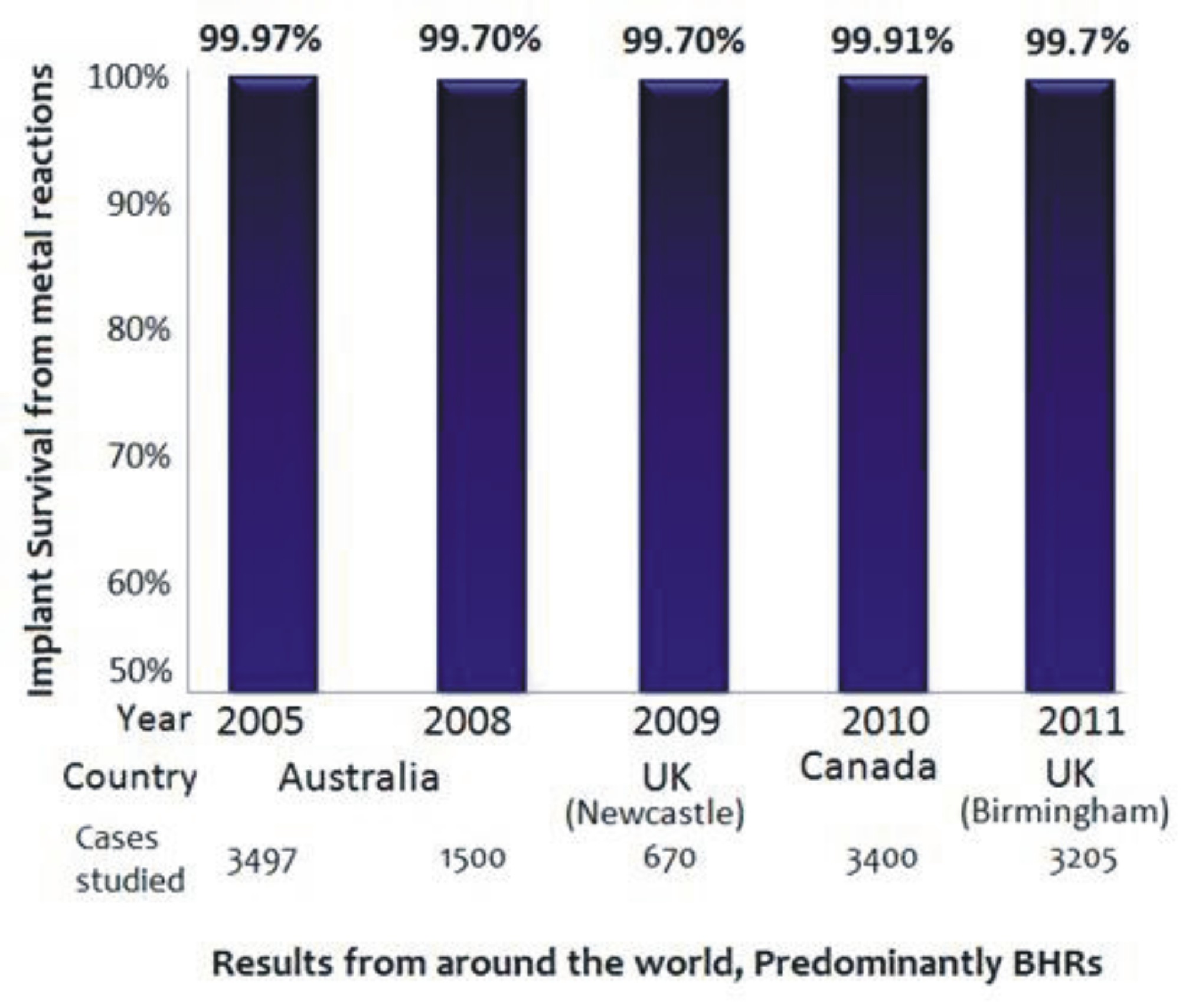
In comparison to the appalling 7‐year results of the ASR, several large series from around the world published 8 to 13 years after BHR introduction confirm a low failure rate from metal debris reactions. The majority of cases in these series were BHRs.
When I received my hip resurfacing, was I treated as a guinea pig or was there sufficient testing beforehand?
There is a perception that all metal‐on‐metal (MoM) resurfacing devices have been introduced into clinical usage without much thought or testing. That is true for many recently introduced resurfacings, but not true for the BHR.
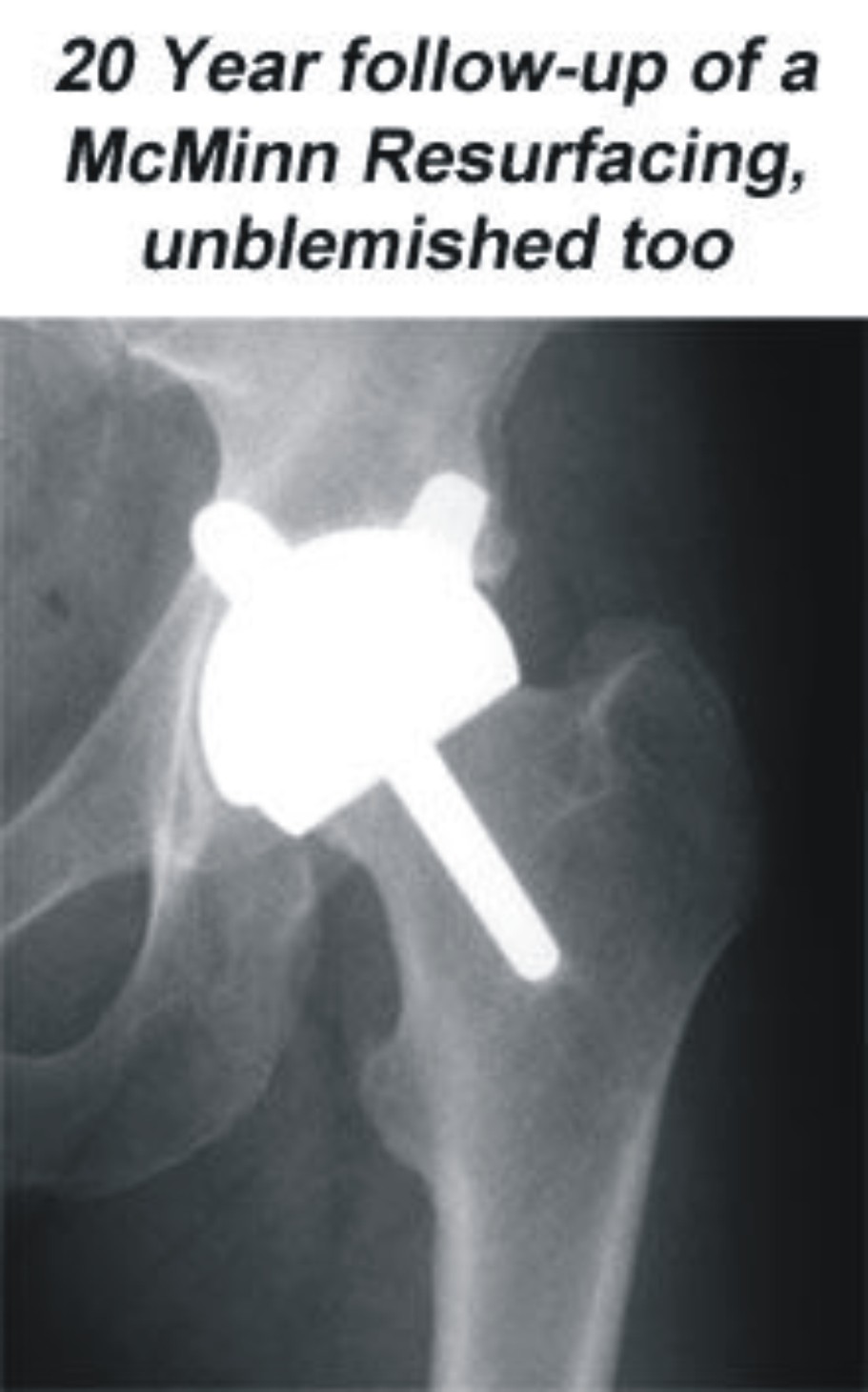
It is 3 months since we at the McMinn Centre celebrated the 20th anniversary of the first modern MoM resurfacing. Since then we have reviewed several patients for their 20‐year follow‐up and some of those early devices are still functioning well.
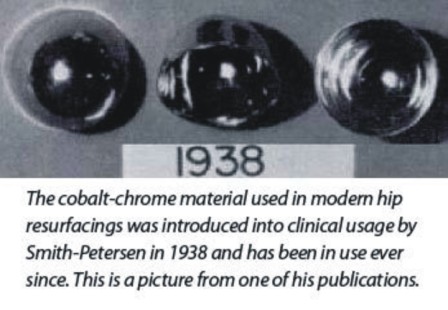
Mr McMinn obtained some of the successful metal components and had them carefully analyzed. Their beneficial design
features and materials were incorporated into my earliest concept models. After further tests we implanted the first modern metal‐on‐metal (MoM) resurfacing in February 1991.
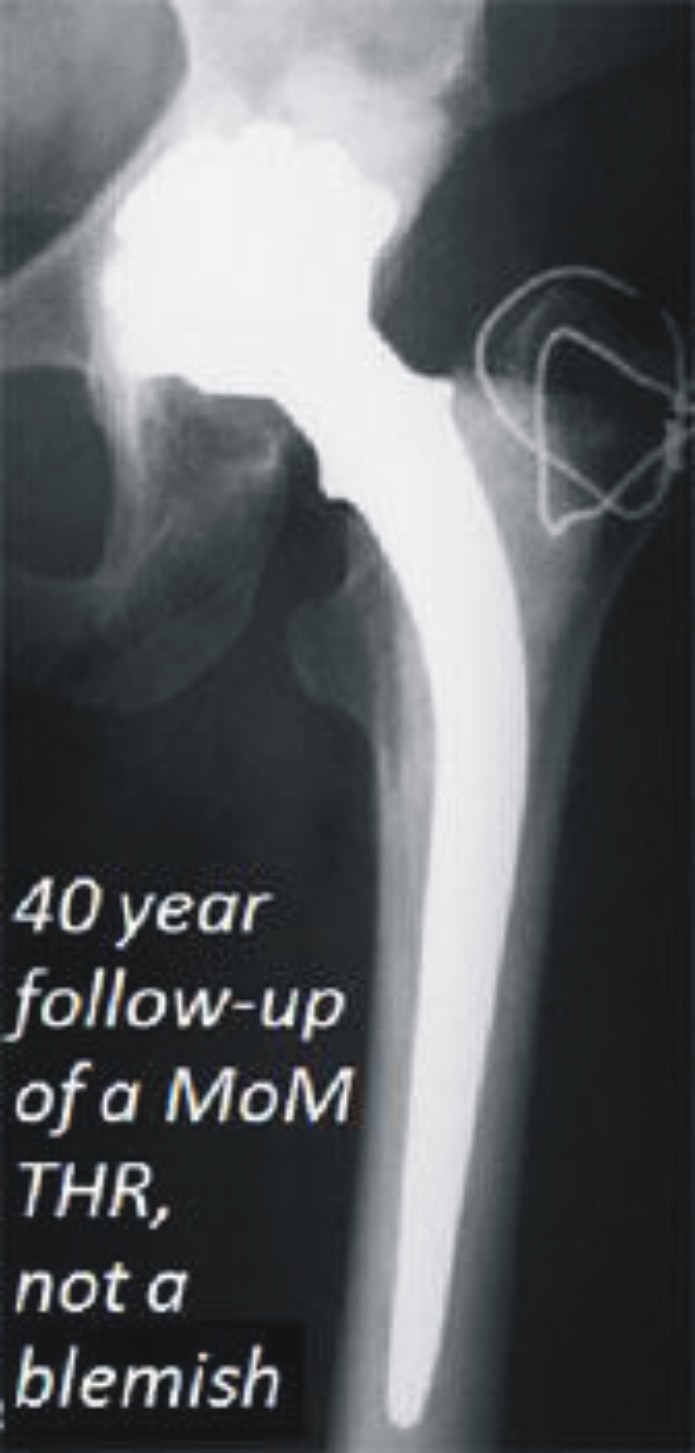
During the next six years we conducted several studies to assess the viability of the femoral head after resurfacing, to determine the best method of fixation of the implants and the effects of metal wear. Further potential problems with the design and material processing of these devices were meticulously identified and addressed in subsequent models, until the introduction of the Birmingham Hip Resurfacing (BHR) in 1997 as a product based on the many lessons learnt during those years.
From 1991 to 1997 the device had largely been used by a few of us hip surgeons in Birmingham and not released for general usage. We had worked on the device in Birmingham for over 6 years and perfected it in a steady stepwise manner before releasing it for general use
After the BHR was introduced, a training program was instituted for surgeons and further studies were started. These relate to hip function, metal ions, implant migration, stress shielding, the effects of resurfacing and replacement on the coagulation cascade and the best form of thromboprophylaxis, to name a few.

I have had a Birmingham Hip Resurfacing (BHR) a few years ago. Other than the odd stiffness and ache I do not experience any symptoms. Do I need metal ion testing?
We have tested hundreds of patients with one‐sided and two‐sided resurfacings and hip replacements. Of the first 350 BHRs we tested all those who could attend a review and provide blood for testing at their 10 year review. There have been no alarming metal ion levels that could cause concern in any. The metal ion levels are in the order of a few parts per billion and at these low levels testing can be tricky. Undertaking these tests at any local laboratory can lead to misleading conclusions. Experts agree that routine metal ion testing is not required except in devices such as the ASR or in very badly positioned components. With a proven resurfacing like the BHR when it is implanted in a good position the wear from the bearing is very low and the prospect of long‐term success is high.
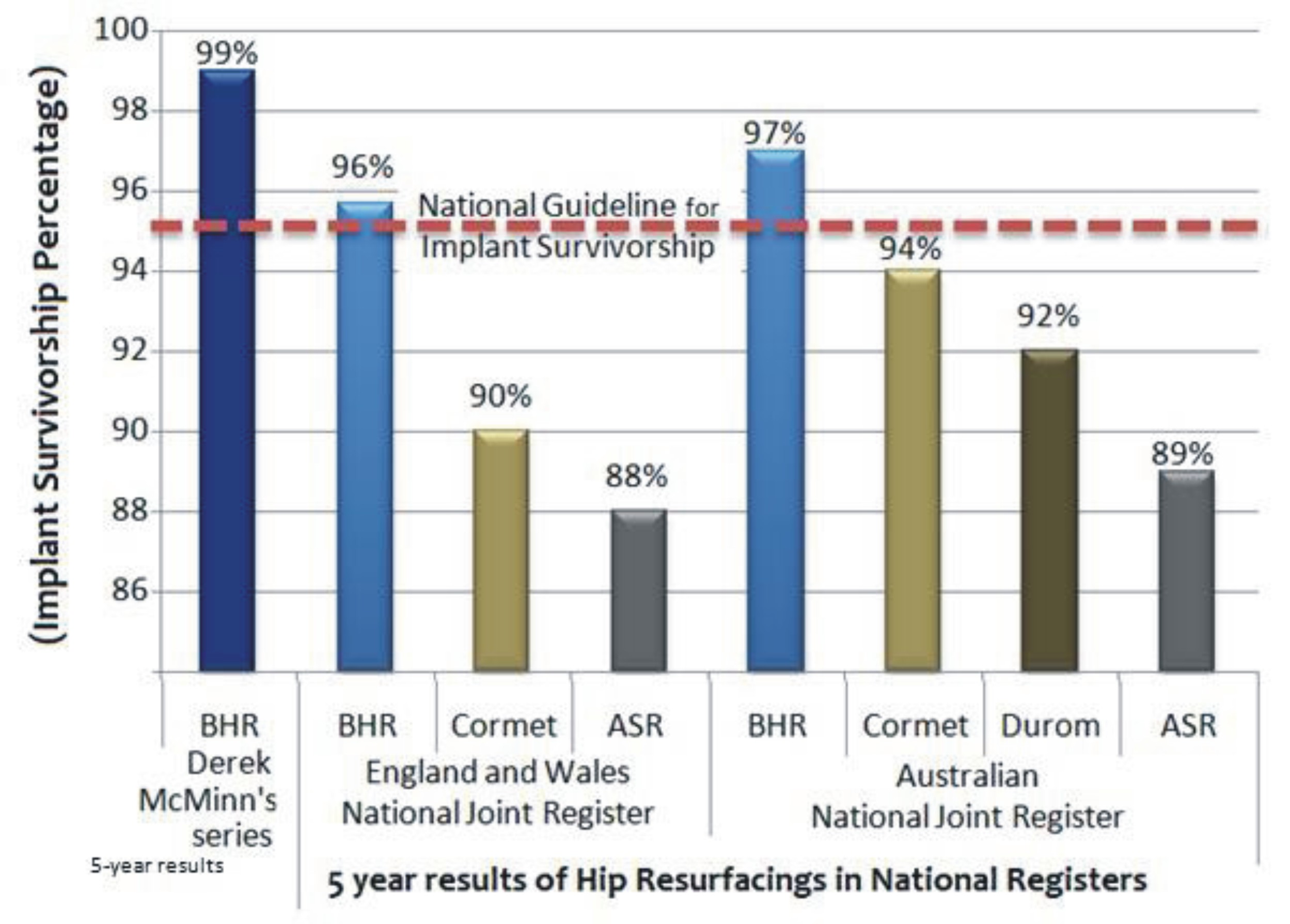
What are the current results of the BHR in the National Joint Registers?
The Australian and the UK National Joint Registers together comprise the largest unbiased documentation of artificial joint devices in the world. The BHR has the longest follow‐up and the largest number of resurfacing cases included in both these Registers. Both these Registers show that BHRs are performing better than the national guideline for excellence in hip replacements.
What then are the options for a young patient with hip arthritis? Are non‐metal‐on‐metal (non‐MOM) hip replacements safer than metal‐on‐metal (MoM) hip resurfacings?
The reason for our introduction of MoM resurfacings in young patients was because the failure rates of traditional hip replacements in the young were very high. The Swedish Register showed that in men with osteoarthritis under the age of 55 years, traditional hip replacements failed at the alarmingly high rate of 19% at 10 years and 67% at 16 years. This is worse than the revision rate of all resurfacings combined and much worse than the revision rates of the BHR in the UK and Australian Registers. These traditional hip failures were associated with much bone loss and progressively difficult revision operations. Our failure rate with the BHR in the same age group and diagnosis is 2% at 13 years.
There are no easy solutions for the young patient. With traditional hip replacements, the problems of multiple revisions and of multiple dislocations in active young patients can be very restrictive for a patient wanting to resume an active lifestyle.
Furthermore every hip device whether using a polyethylene bearing or a ceramic bearing has metal in the stem and/or in the cup. It is just coming to light that with non‐MoM hips also can leech metal from the (taper) joint connecting the stem and the head (or the cup and the insert) and cause the same problems as seen with bad resurfacings.
What has shocked many in the orthopaedic community is a hitherto unidentified finding in the UK National Register that the mortality rate 5 years following hip resurfacing is phenomenally lower (1.8%) compared to that following hip replacements (9.9%). This benefit persists even after adjustment for age, gender and physical status. This suggests that traditional hip replacement adds some as yet unidentified detrimental effect to the patient as a whole, which the recipients of hip resurfacing appear to escape.
SUMMARY
Total hip replacement in young patients comes with the price tag of a higher revision rate and a higher mortality rate. A well‐designed, well‐engineered, well‐implanted resurfacing is a much better option than a hip replacement.
There is now overwhelming evidence which clearly shows that ASR was a badly designed resurfacing. The same evidence also demonstrates that the results of the BHR in young patients are very good, the very group who fare poorly with a traditional hip replacement. It would be unfortunate if the bad results from a few ill‐designed, poorly implanted devices are allowed to throw this excellent treatment option into disrepute.
The BHR has been implanted in more than 140,000 patients worldwide. It has restored quality of life and returned young patients to their professions. One study found that over 90% of the resurfaced men participated in sporting activities and over 60% participated in impact sports without detriment to their artificial hip. As the inventor of the BHR, Mr McMinn is confident that this technology will stand the test of time as the published< evidence has been proving.
It must be remembered however that component malposition is a cause of failure and should be avoided.
Choose your device and your surgeon carefully. If you have any further queries, please do not hesitate to contact
us: enquiries@mcminncentre.co.uk
Joseph Daniel FRCS MS(Orth)
Director of Research at The McMinn Centre
May 2011