Dr. Gross - What type of femoral fixation is better, bone in growth or cement?
Thomas P Gross 7/12/2022
Uncemented fixation appears to be superior. Using the Zimmer Biomet Recap magnum system, we compared [1] cement to bone ingrowth fixation of the femoral component. Late femoral loosening occurred in 0.9% of cemented components and in no uncemented components. My current 15-year implant survivorship is 99% in over 5000 cases of Recap/Magnum uncemented Hip resurfacing. This means a 1% cumulative failure rate by 15 years due to all failure modes. If I had used cement, my previous study would predict that my failure rate would at least double to 2%. In my comparison study, the early femoral failure rate (femoral neck fracture or femoral head collapse prior to 2 years) was also lower (0.4% vs 0.9%) with bone ingrowth than cement fixation. But this may have been due to improvements in postoperative management protocols rather than the method of fixation. The difference in late femoral fixation failure (after 2 years) from 0.9% to 0 was highly significant (p<0.0001). This demonstrates that at least for the Recap/magnum system uncemented femoral fixation is superior.
All Hip resurfacings have an uncemented (porous, bone ingrowth) socket. There is no disagreement that this is the superior fixation method for the acetabular component. Most Hip resurfacing systems have a cemented femoral component. The Recap/Magnum metal-metal implant that I use, and Jim Pritchett’s new metal-poly implant (no published data) are both completely porous. Systems that employ both cement and porous are termed hybrid systems. All other systems are hybrid, there are no completely cemented systems.
From a theoretical standpoint, cement offers immediate fixation but kills some bone in the exothermic curing process. Late failure can occur due to cement fatigue. Porous fixation requires an initial tight press fit and time for ingrowth. The theoretical problem would be failure of in growth. Surprisingly, this has never occurred in my experience (over 6000 porous cases). Once ingrown, porous coating is more durable than cement.
On the other hand, cement actually works much better on the femoral component than I predicted 20 years ago. The cement in a femoral resurfacing is generally loaded in compression which is favorable for cement. Cement fixation in resurfacing has therefore done much better than cement in total hips and total knees.
Cement seems to work especially well if the femoral head bone is hard and there are no large defects. If the bone defects are cavitary and can be filled with bone graft and cemented over, the outcome is better than if the defect is filled with exothermic cement. In osteonecrosis[2] the defects tend to be segmental which makes it hard to use this grafting technique, so the outcome is worse. In osteoporotic bone the cement also penetrates more deeply into the bone and burns more bone causing more failures. That is why McMinn has more failures in older women. In summary, cement works best in hard bone and with contained defects that are grafted.
The BHR is only available with cement fixation for the femoral component. Proponents of this system have in the past provided many theoretical reasons why cement is superior. I can provide many reasons why uncemented might be superior. We are now past the point where theoretical reasons matter anymore. Data is now available to decide the question. At this point in time, I have the only published comparative study of femoral fixation [1]and it demonstrates that for the Recap/Magnum system bone ingrowth is superior. This, of course, may not necessarily apply to all systems; design specifics are very important. It is possible that if Smith Nephew Richards (SNR) released a porous Birmingham Hip resurfacing (BHR) femoral component, it might not work as well as their cemented version. I have established that for the Recap/Magnum system, porous is superior.
It is true that the SNR BHR is the most widely used worldwide and has excellent outcome from many centers. I am the only surgeon to extensively use the Recap/Magnum system and publish data on it. So how does the Recap/Magnum system stack up to the BHR for overall results? Also the Wright Medical Conserve has a long track record with the late Amstutz and also DeSmet.
I am currently working on a publication of 15-year data with the Zimmer Biomet Recap/Magnum system. Here is the comparison table from our work in progress:
Table 8. Literature Comparison
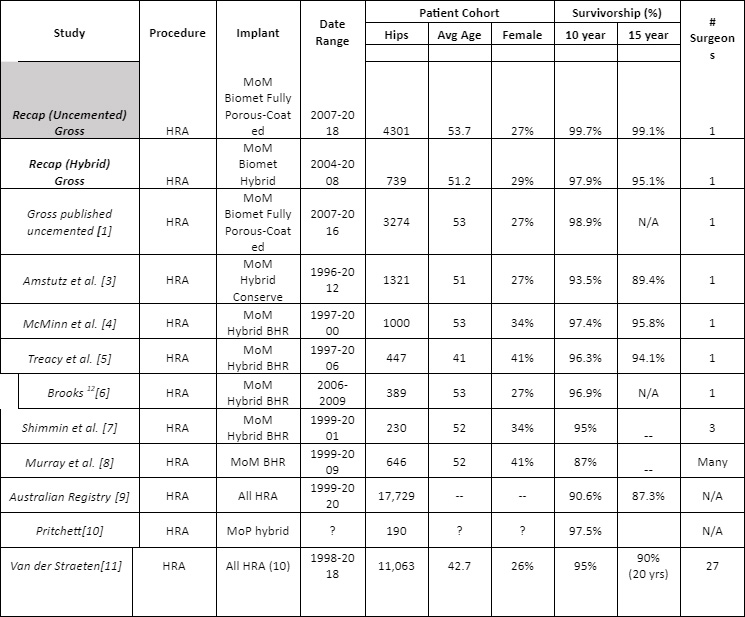
MoM=metal-on-metal
Hybrid=femoral fixation cement / acetabular uncemented
Porous fixation is technically easier, works in all cases, can be used in cases with extensive bone loss, and carries the theoretical advantage for long-term fixation well beyond 10 years.
Although the BHR has an excellent track record, if you use it you do have to accept a slightly higher long-term failure rate due to cement and you cannot resurface smaller patients and women. It is FDA approved for marketing as a Hip resurfacing device but is now labeled to avoid use in women. Several years ago, they stopped selling all bearing sizes smaller than 48mm.
If you use the Recap/Magnum, porous fixation allows an improved long-term outcome at 15-years, but virtually all data is derived from one high volume surgeon. The implants are FDA approved but are used off-label for Hip resurfacing. Please look up what this means in Wikipedia.
In the Recap/Magnum system all implant sizes are available, and there is no legally charged labeling warning against use in women. I can resurface women and smaller men who I believe have a right to choose hip resurfacing. My outcomes in these groups in the past were slightly inferior to those of large men, but still better than results for THR. In the last 10 years results are now identical for both sexes, all implant sizes, all diagnoses, and all ages. Most published BHR results are inferior in women and smaller sizes, but I do not believe this is an inherent problem of the implant (as the manufacturers behavior implies), but rather it is a matter of technique[12].
Currently my 15-year implant survivorship is 99% with fully porous Zimmer Biomet Recap/Magnum metal-metal Hip resurfacing in over 5000 cases. I do not exclude people based on age, sex, diagnosis, or implant size. I resurface heads with up to 50% bone loss in younger patients.
I believe the Biomet Recap uncemented system now appears to be the best on the market. It is now important for other surgeons to verify this with their own data.
All the references below that I have authored are available for more close review on my website grossortho.com/ patient education/ scientific publications. Others can be obtained for a fee by searching pub med.
- Gaillard-Campbell, D.M. and T.P. Gross, Femoral Fixation Methods in Hip Resurfacing Arthroplasty: An 11-Year Retrospective Comparison of 4013 Cases. J Arthroplasty, 2019. 34(10): p. 2398-2405.
- O'Leary, R.J., M.D. Gaillard, and T.P. Gross, Comparison of Cemented and Bone Ingrowth Fixation Methods in Hip Resurfacing for Osteonecrosis. J Arthroplasty, 2017. 32(2): p. 437-446.
- Amstutz, H.C. and M.J. Le Duff, The mean ten-year results of metal-on-metal hybrid hip resurfacing arthroplasty. Bone Joint J, 2018. 100-B(11): p. 1424-1433.
- Daniel, J., et al., Results of Birmingham hip resurfacing at 12 to 15 years: a single-surgeon series. Bone Joint J, 2014. 96-B(10): p. 1298-306.
- Matharu, G.S., et al., The outcome of the Birmingham Hip Resurfacing in patients aged < 50 years up to 14 years post-operatively. Bone Joint J, 2013. 95-B(9): p. 1172-7.
- Samuel, L.T., et al., Hip Resurfacing: A Single Surgeon U.S. Series With Minimum Ten-Year Follow-up. J Arthroplasty, 2022.
- Coulter, G., et al., Birmingham hip resurfacing at a mean of ten years: results from an independent centre. J Bone Joint Surg Br, 2012. 94(3): p. 315-21.
- Murray, D.W., et al., The ten-year survival of the Birmingham hip resurfacing: an independent series. J Bone Joint Surg Br, 2012. 94(9): p. 1180-6.
- Association, A.O., Australian Orthopaedic Association National Joint Replacement Registry. 2021.
- Pritchett, J.W., Hip Resurfacing Using Highly Cross-linked Polyethylene : Prospective Study Results at 8 . 5 Years. The Journal of Arthroplasty, 2016. 31(10): p. 2203-2208.
- Van Der Straeten, C., International hip Resurfacing Group, Hip resurfacing arthroplasty in young patients: international high-volume centres’ report on the outcome of 11,382 metal-on-metal hip resurfacing arthroplasties in patients < 50 years at surgery. HIP International, 2020: p. 1-10.
- Gross, T.P., Hip resurfacing: is female gender an absolute or relative contraindication? Annals of Joint, 2021. 6: p. 23-23.
